Racial profiling
What is racial profiling? Provide examples of how law enforcement, government officials and/or ordinary citizens use racial profiling in the aftermath of 9/11. (review Arizona case). How might the contact hypothesis remedy profiling?
Sample Answer
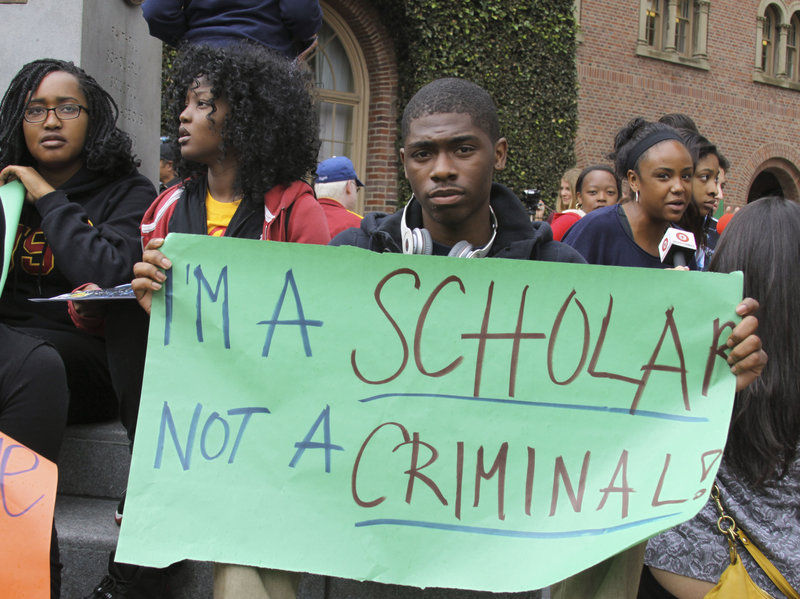
According to Americas Civil liberties union (capitals ACLU) the concept of racial profiling refers to the practice by law enforcement officials of targeting individuals for suspicion of crime based on the individual’s race and natural origin. of racial profiling occurs where there are deviations from established laws, an indigenous person is singled out just on account of his skin color and are subjected to degrading treatment. Racial profiling can be renegade through policy frameworks, engagement, organization change, collection and acknowledgement.
The blood glucose level is controlled as a feature of metabolic homeostasis (Young, 1977). The ordinary scope of glucose in the plasma is managed between 3.5-8.0 mM (Arciero et al., 1999). The degree of the sugar in the blood outside the ordinary range might be characteristic of an ailment. A constantly elevated level in blood glucose is alluded to as hyperglycemia and low glucose levels are alluded to as hypoglycemia (Colberg and Colberg, 2009; Lee et al., 2005). Glucose shipped from the digestion tracts or liver to the body cells is made accessible for take-up by assimilation cells and digestion (Reddy, 2012).
The islets of Langerhans in the pancreas arranges the discharge of insulin and glucagon (Lowell and Shulman, 2005; Quesada et al., 2008). If the blood glucose levels rise the ß-cells import and oxidize glucose to help mitochondrial ATP blend. This procedure animate an ascent in the cytoplasmic ATP/ADP proportion, which thusly instigates the Ca2+ take-up from mitochondria pursued by an arrival of insulin (Maechler et al., 2010; MacDonald et al., 2005). After its discharge the insulin guarantees the take-up of glucose from delicate tissues, digestion and capacity of glucose as glycogen or lipids. Insulin can neutralize the impacts of glucagon in the liver. This happens by restraint of gluconeogenesis and glycogenolysis. Low blood glucose levels brief the discharge of glucagon which thus instigates glyconeogenesis and glucose assembly in the hepatic tissue. These procedures at that point reestablishes euglycemia and at the principle time counteract insulin activity (Quesada et al., 2008).
If there is an interruption in the planned discharge of insulin and glucagon, it might prompt enduring obsessive impacts, including the improvement of type1 diabetes (T1DM) and type2 diabetes (T2DM). Both T1DM and T2DM are portrayed by continuous disappointment and devastation of the ß-cells. T2DM creates through an unpredictable transaction among hereditary qualities and natural factors, for example, presentation to poisons, diet and liquor utilization (Cnop et al., 2005). T1DM is portrayed by an auto-safe ambush, which happens with the intrusion of the islets by mononuclear cells and enlistment of intra-islet irritation and cell apoptosis (Knip et al., 2005). Improvement of T1DM can likewise be encouraged by presentation to synthetic concoctions. Synthetic substances, for example, alloxan and streptozotocin are frequently regulated to specifically annihilate ß cells and incite T1DM. The two compound substances kill ß cells by instigating oxidative pressure and harm by disturbing pancreatic particle transport and calcium levels (Szkudelski, 2001).
The significant wellspring of blood glucose is dietary sugars, for example, starch, which are hydrolyzed by a-glucosidases and pancreatic a-amylase, in order to be consumed by the small digestive tract. Inhibitors of the proteins could hinder the take-up of dietary starches, which stifle postprandial hyperglycaemia. Alpha-glucosidase inhibitors, for example, acarbose, miglitol, and voglibose are known to limit postprandial hyperglycemia fundamentally by meddling with the action of starch processing catalysts and decline glucose ingestion (Maurus et al., 2005).
Hypoxis hemerocallidea (HH) is one of the most usually utilized therapeutic plants in South Africa (Nair et al., 2007). It is utilized for the treatment of various afflictions which incorporate urinary tract contaminations, coronary illness, fruitlessness and tension (Brown et al., 2008). Because of its helpfulness in customary drug, Hypoxis hemerocallidea has pulled in a great deal of enthusiasm for logical investigations (Nair et al., 2007). Hypoxis concentrates contain phytosterols which are believed to be the fundamental pharmacological fixing answerable for its enemy of lipidemic, hostile to diabetic and mitigating properties (Boukes et al., 2008). A fluid concentrate of Hypoxis hemerocallidea was found to show a noteworthy decrease in the blood glucose levels of fasted typical and Streptozotocin (STZ) actuated diabetic rodents (Mahomed and Ojewole, 2003). It is felt that the blood glucose bringing impact watched is expected down to the nearness of phytosterols or potentially sterolin. The component of the blood glucose bringing down activity is as yet not surely known. Ojewole (2006) in an investigation wherein a fluid concentrates of Hypoxis hemerocallidea were orally managed discovered enemy of diabetic impacts beginning at 100 mg/kg in both normoglycaemic and hypoglycaemic rodents.
1.1 The reason for the examination
The plant Hypoxis hemerocallidea, otherwise called the African potato, is normally utilized as a customary medication to treat diabetes in South Africa. There are numerous components that prompting low blood glucose level, and one of these instruments is increment insulin emission. The motivation behind this examination is along these lines to investigate the impact of Hypoxis hemerocallidea on insulin discharge and processing chemicals.
1.1.1 Specific destinations
• To decide the potential danger of Hypoxis hemerocallidea and glucose on pancreatic RIN5-F cell suitability
• To decide if Hypoxis hemerocallidea can build insulin emission from the pancreatic RIN5-F.
• To decide if Hypoxis hemerocallidea can repress the action of a-amylase and a - glucosidase.
Part II
2 Literature audit
The body normally controls blood glucose levels as a feature of metabolic homeostasis (Young, 1977). The glucose is consumed by the digestion tracts and discharged into the blood (Magistretti and Pellerin, 1999; Miller et al., 1995). Notwithstanding the body circumstance, for example, starvation, extraordinary physical exercises and admission of enormous amounts of nourishment, the typical degree of glucose in the plasma is 3.5-8.0 mmol/L. (Arciero et al., 1999). To control glucose, the body has three hormones: glucagon, insulin and epinephrine (Lotfy, 2012). The degree of the sugar in the blood outside the ordinary range might be a marker of an ailment. A determinedly high blood glucose are sent to as hyperglycemia and low levels in glucose are alluded to as hypoglycaemia and (typically under 3.5 mmol/L) (Colberg and Colberg, 2009; Lee et al., 2005).
Normally the glucose is gotten from 2 sources, the intestinal retention that pursues the assimilation of sugars nourishment and glucose discharged into the dissemination from the kidney and liver after gluconeogenesis process (Giugliano et al., 2008). Glucose is shipped from the digestive organs or liver to body cells by means of the blood, and is made accessible for take-up by the cells (Reddy, 2012). Glucose levels are typically least in the first part of the day prior to the principal supper of the day and ascend after dinners for an hour or two by a couple millimolar (Colberg and Colberg, 2009; Reddy, 2012). Glucose digestion systems occur in the muscles and liver (König et al., 2012). The activity that by which straightforward sugars found in numerous nourishments are handled and used to deliver vitality as ATP (Magistretti and Pellerin, 1999; Miller et al., 1995).The glucose assimilation by various body tissues happens under the impact of two elements which are the openness of glucose and the physiological states of the tissue. These two frameworks wherein glucose retention happen are streamline transport (a latent way) down the glucose focus relapse, and optional dynamic dispersion against glucose fixation relapse (a functioning aberrant way that needs adenosine triphosphate (ATP), as root of vitality). (Lotfy, 2012).
There is two hormones discharged from the pancreas are for the most part answerable for blood glucose guideline, insulin and glucagon, insulin is the predominant glucoregulatory hormone, which direct the blood glucose level in the fasting state (Rizza et al., 1985). While the glucagon considered as an intense hyperglycemic hormone, which is work solely on the liver to lift hepatic glucose creation inside minutes. Ingestion of starch inspires a quick ascent in insulin fixation and a decrease in glucagon focus. The expansion in insulin focuses occur before raising the blood glucose fixations is believed to be interceded to a great extent by hormonal sign emerging in the stomach related framework (Aronoff et al., 2004; Kuznetsov, 1978).
2.1 The Pancreas and blood glucose level control
The pancreas is a glandular organ in the upper piece of the stomach area, however fills in as two organs in one: a stomach related exocrine organ and a hormone-creating endocrine organ. Functioning as an exocrine organ, the pancreas secretes catalysts to crush the lipids, proteins and starches in nutriment (Olubummo, 2010). It weighs between 70 g and 110 g (Gromada et al., 2007; Nobukawa, 2007). The pancreas is connected to the duodenum, the initial segment of the small digestive tract by means of the regular pancreatic bile pipe. The organ is likewise reached out towards the spleen (Figure 2.1.).
The Langerhans islets (Figure 2.2.) comprising of insulin discharging ß-cells (65-90 %) shaping the center of the islet, glucagon-discharging alpha-cells (15-20 %) (Zhou et al., 2011), pancreatic polypeptide cells creating (1 %) PP and somatostatin-delivering delta-cells (3-10 %), generalley it situated superficially (Elayat et al., 1995). ß-cells, which couple supplements digestion with electrical action to regulate the produce and arrival of insulin, have been more often than not considered. The islets of Langerhans assume a significant job in glucose digestion and sort out of blood glucose fixation (Jo et al., 2007).